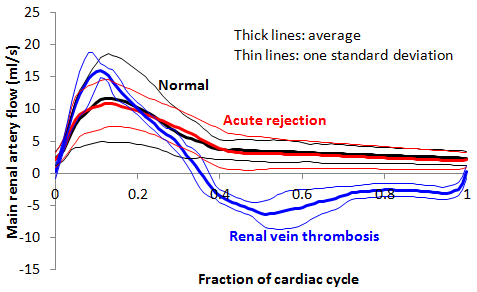
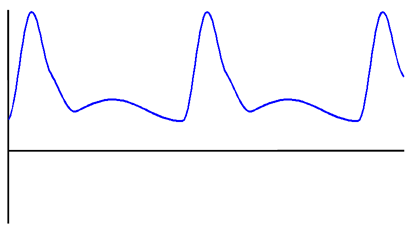
Figure A: Average renal artery waveforms in normal kidney transplants, acute rejection, and renal vein thrombosis.
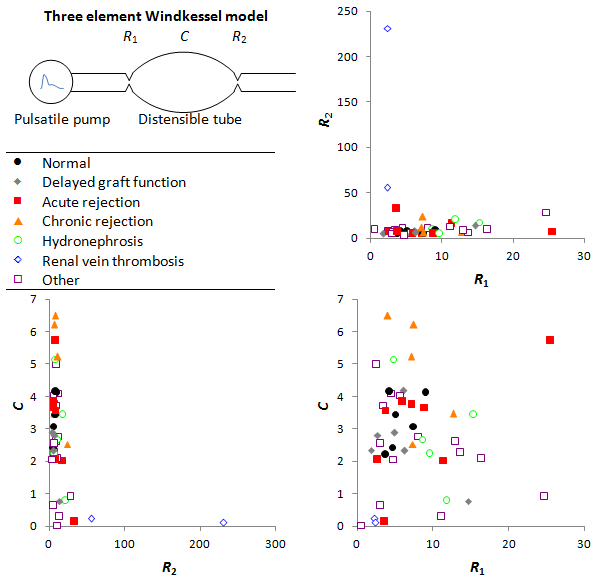
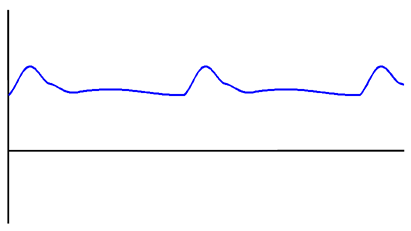
Figure B: Pre- and post-glomerular resistance and vascular compliance for each diagnosis.
Purpose: Doppler ultrasound resistive index (RI) is a widely used parameter in the assessment of renal transplant function, but current work suggests that its sensitivity and specificity for acute rejection is low. Although RI (which is a measure of pulsatile flow) does increase with post-glomerular vascular resistance, it also increases with increased vascular compliance (decreased atherosclerosis), decreased pre-glomerular vascular resistance, increased pulse pressure, and increased heart rate. We postulated that separating out these potentially confounding factors and directly calculating vascular resistance and compliance, would allow for more accurate assessment of kidney transplants.
Materials and methods: 47 kidney transplant ultrasounds were analyzed. RI was measured at the segmental renal arteries. We modeled the transplanted kidney vasculature as a tube with a pre-glomerular and post-glomerular vascular resistance, and a vascular compliance (three-element Windkessel model). This model accurately describes in vivo blood flow in rat kidneys. The arterial blood pressure was modeled using a range of waveforms from the MGH/MF Waveform Database, adjusted to match the patient's measured heart rate, systolic blood pressure, and diastolic blood pressure. The parameters of the model were adjusted to fit the experimental mid renal artery velocity waveforms. The final diagnosis was determined from pathology (when available) and the nephrology clinic visit notes.
Results: Normal transplant kidneys have an average RI of 0.71 ± 0.11, and kidneys in acute rejection have an RI of 0.77 ± 0.11. Using a cutoff of 0.8 results in a sensitivity of 38% and specificity of 63% for acute rejection. A resistive index > 1 was only seen in renal vein thrombosis (2 cases). Waveforms for acute rejection, chronic rejection, hydronephrosis, and delayed graft function all had a large amount of overlap with normal waveforms (Figure A). Using the three-element Windkessel model, we showed that these 4 diagnoses are associated with vascular resistances and compliances within 1 standard deviation of normal, and none of the differences were statistically significant (Figure B). On the other hand, renal vein thrombosis is associated with a non-significant increase in post-glomerular resistance, and a significant decreases in pre-glomerular resistance (p=0.01) and vascular compliance (p=0.0003).
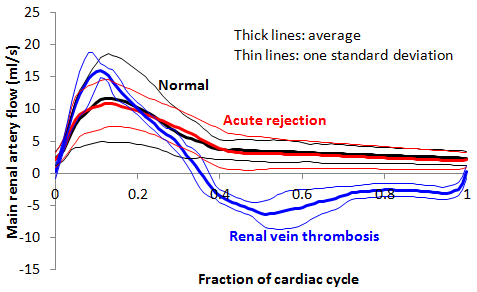
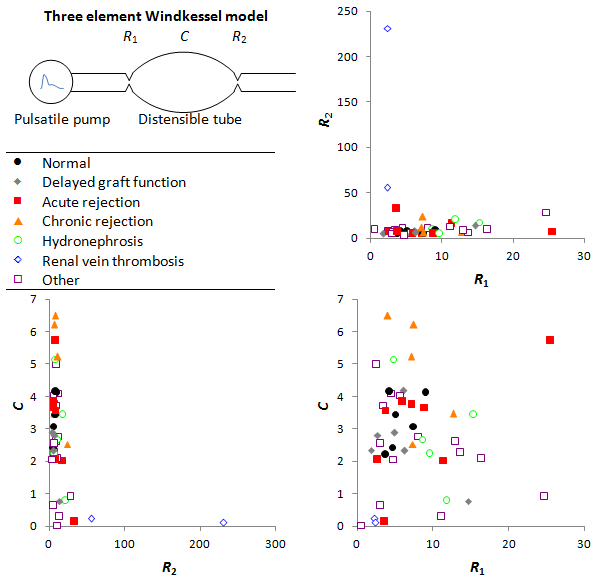
Figure B: Pre- and post-glomerular resistance and vascular compliance for each diagnosis.
| Normal | Decreased vascular compliance (C) |
 |  |
|
|
| Increased pre-glomerular resistance (R1) | Increased post-glomerular resistance (R2) |
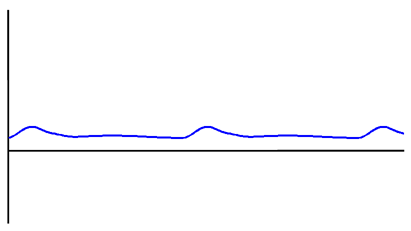 | 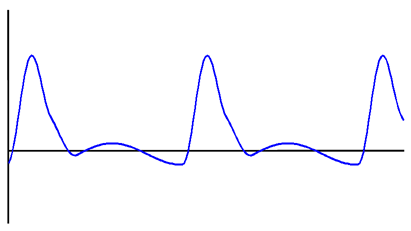 |
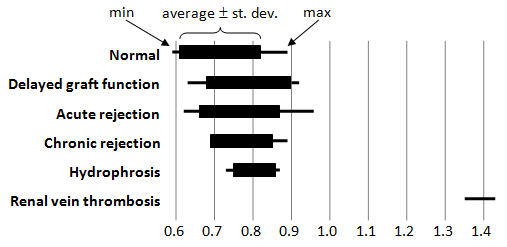
Figure D: Intra-renal resistive index for each diagnosis.